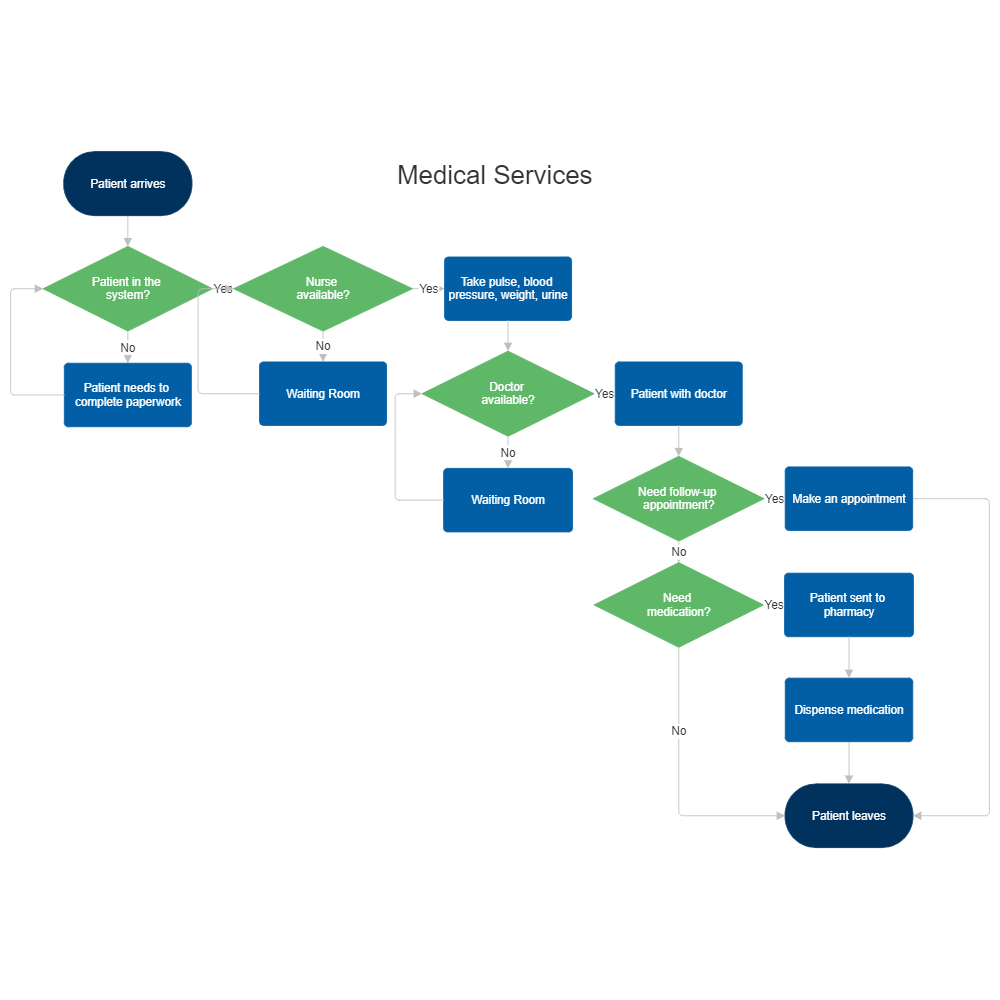
Case Management Utilization Review Process Flowchart
Is there inter rater reliability testing and quality assurance of case utilization management.
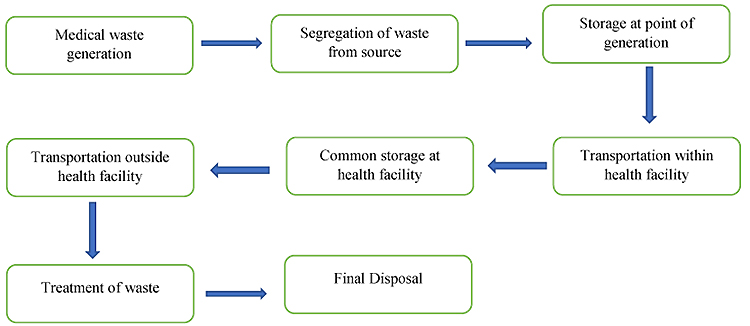
Case management utilization review process flowchart. It is also true that the goal for both is to control the cost of healthcare services. Is the medical necessity admission review process in effect 7 days per week 365 days per year. Introduction case management is a malleable and easily adapted model that applies to a variety of care delivery locations and systems. This includes medical necessity continued stay level of care potential delays in care and progression of care.
On the other. Critical case management functions during the admission phase include admission review for medical necessity and appropriate patient class using standardized inpatient utilization criteria. This course gives nurses and case managers general working knowledge of what utilization management utilization review is including the definition process insurance principles and related laws. Discharge planners work on each unit in the hospital and have a caseload of anywhere from 30 40 patients.
The complete utilization review process consists of precertification continued stay review and transition of care. It is true that the evaluation process for utilization review and utilization management is similar or the same and both assess medical care for appropriateness. Piloting quality improvement initiatives focused on readmission reduction care coordination through better communication and population health management. Utilization management ensures services provided are medically necessary and provided at the appropriate and least costly level of care.
Case management of adults and utilization management for adults and children are delegated to. When a patient is admitted to the facility a first level review is conducted for appropriateness. Is there ongoing training and education available for case utilization management and physician advisor teams. Discharge planning and utilization review.
The terms utilization review and utilization management are often used interchangeably. Although case management has been used in the community setting for the longest period it is now commonly seen as an integrated care. Where i work case management is split into two divisions. They do case management evaluations on each patient and make all discharge arrangements i e transfers to skilled nursing alf s arrange for home o2 walkers canes etc.
These traits have enabled organizations applying the model to design and implement the model to meet their specific needs.